Periodontitis is due to persistent subgingival BIOFILM within TARTER (barnacles).
‘Biofilm-related infection’ is very different than any soft tissue (i.e. skin) infection. Different bacteria within biofilm survive by metabolic cooperation and works towards survival of the “community” (biofilm).
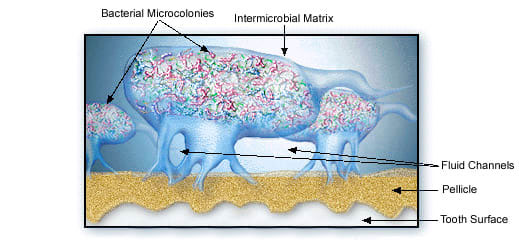
The biofilm cannot be removed by only mouthwash or only antibiotics due to sticky matrix surrounding the micro-organisms protecting the “bugs” against antibiotics and mouthwashes. The good bugs with antibiotic resistance can also protect bad bugs without any resistance! Additionally mouthwashes don’t penetrate enough in the pocket (gap between gums and teeth) to work against biofilm.
Effective control of biofilm cannot be achieved by:
Removal of biofilm below the gum line is required to subside the damaging inflammatory response.
Periodontitis inflammation/infection is largely controlled with nonsurgical periodontal therapy.
Nonsurgical periodontal therapy is comprehensive, meticulous approach of removing plaque and tarter from below gum line, without cutting the gums.
Success of nonsurgical periodontal therapy relies on:
Based on our extensive experience at Perio’Plant, in combination with special tools and methods we implement, we can assure most of our patients with severe disease, during the initial assessment, about the teeth that would respond well to nonsurgical periodontal therapy.
In a small fraction of teeth, we further recommend periodontal regeneration.
An example of advanced periodontal treatment using growth factors to stimulate periodontal regeneration:
At Perio’Plant we provide patient-specific solution with least invasive intervention and minimum associated morbidity (pain, swelling, etc.).
Periodontitis inflammation below gingival area, when placed together, represents “palm size” ulcer. Constant exposure to microbial biofilm and bacterial toxins over a time in the body can have some negative health effects over a long time.
Years of systematic research suggest a link of untreated periodontitis with at the least:
Diabetes additionally makes periodontitis worse, and periodontitis worsens diabetes – the sugar (glycaemic) control leading to double-edge sword or two-way relationship.